How Medicaid Leaders are Preparing for HR1: Operational Readiness at Scale

Two conversations at Medicaid Innovations - one focused on Medicaid renewals, the other on HR1 implementation - kept circling the same realization: this is not an eligibility redetermination story. It’s a sustained compliance, verification, and communications challenge, landing on systems that are already under pressure.
As Jennifer Strohecker, PharmD (President, Strohecker Health Solutions and former Medicaid Director in Utah), framed it at the outset, states are facing a compressed timeline where work requirements and six-month eligibility reviews arrive at the same time… and then continue indefinitely. “It’s different than unwinding,” she noted. “It doesn’t stop.”
That distinction shaped everything that followed.
1. HR1 is landing on top of renewal backlog - but not on empty operations
States are entering this next phase with real constraints, but also real operational muscle.
Sarah Spiekermeier, Interim CEO and Executive Director of Medicaid at Banner Health Plans, shared that her state of Arizona is already 60,000 renewals behind. At the same time, she was clear that they are not starting from scratch. Her team already runs regular “Medicaid scrubs” that intentionally bring together employment, housing, and other functional teams (outside of their silos) to identify issues and resolve them collaboratively.
What’s changing now is the need to formalize and scale that coordination. Sarah described evolving toward an integrated vital documents program that builds on existing teams and workflows, rather than creating parallel processes that risk duplicative outreach and member confusion.
Theme: The challenge isn’t lack of teams; it’s making cross-team coordination systematic enough to scale.
2. The biggest wins happen before you ever engage a member
One of the strongest throughlines came from Victor Sanchez, Vice President of Business Development at CITIZ3N Government Solutions, who emphasized the importance of upfront pathway design.
Instead of jumping straight to outreach, Victor argued for walking through the entire compliance journey in advance - checkpoint by checkpoint - to identify where people get stuck, which exemptions apply, and where engagement is unnecessary.
“This is not an eligibility play,” he said. “People are already deemed recipients. It’s compliance and requirements.”
Knowing, for example, which exemptions (like medical frailty) are routinely applied can remove large numbers of people from redundant engagement entirely.
Theme: Invest early in understanding the pathway, and you reduce confusion, waste, and churn downstream.
3. Verification will be hybrid, messy, and capacity-constrained
Multiple speakers acknowledged that work and community engagement verification will be far from clean.
Jim Milanowski, CEO of Genesee Health Plan, raised practical concerns about verifying 20-80 hour thresholds at scale, especially for volunteering and internships.
Victor Sanchez reinforced that this complexity is structural, not temporary:
- Gig and nontraditional work will be common
- Participation may fluctuate month to month (school one period, work another)
- Documentation won’t fit neatly into existing boxes
“Organize the chaos,” Victor urged, noting that hybrid reporting and transparency (being able to show how a determination was made) will be unavoidable.
Theme: Systems need to be designed for ambiguity, not edge cases.
4. Mail can’t carry this complexity - relationships have to
If one line stuck with the room, it came from Janet Mann, Director at the Arkansas Department of Human Services:
“Snail mail is dead.”
Arkansas learned during unwinding that phone numbers are the real asset. If the state can text someone, it’s far more likely to keep contact information current and avoid silent failures. Janet described how lessons from unwinding, such as SMS, provider outreach, community partnerships, and social media, are now being rethought as core system behavior, not temporary mitigation.
This matters even more as Arkansas prepares to run six-month redeterminations for expansion adults alongside annual reviews for other populations, all within an integrated eligibility system spanning Medicaid, SNAP, and TANF.
Theme: Multi-channel communication isn’t supplemental; it is the infrastructure.
5. Confusion, not resistance, is what drives churn
From the member perspective, Manny Felix, Sr. Director of Medicaid Sales at Blue Cross Blue Shield of Arizona, described confusion as the dominant theme in listening sessions.
Members often receive multiple notices that appear contradictory:
- one says they’re approved
- another asks for more information
- a third implies further action is required
The result is a common conclusion: “I’m approved, so I don’t need to do anything.”
Manny emphasized that churn is frequently triggered by small, avoidable issues, like a missing signature or misunderstanding which part of a notice matters. Teaching members how to read the notice can be just as impactful as changing the notice itself.
Theme: Clarity beats volume every time.
6. Effective engagement happens during care moments
Several speakers argued that eligibility and compliance work lands best when paired with care - not treated as a separate administrative interaction.
Celina Sullivan, representing Kaiser Permanente, described embedding prompts directly into clinical and operational workflows so receptionists, medical assistants, and physicians can see what a member needs in real time. This includes alerts, risk flags, and proactive outreach supported by data.
Jatin Dave, from UPMC Health Plan, echoed this approach and stressed that moments like prenatal visits, pharmacy encounters, and emergency care are when members are most receptive.
At the same time, he cautioned that HR1 will quickly expose how siloed providers, plans, and states still are.
Theme: Meet people where they already are, especially when health is top of mind.
7. More support isn’t always better; sequencing matters
A quieter but important lesson surfaced across both sessions: don’t overload people.
Speakers repeatedly warned that stacking employment, food, housing, and paperwork referrals at once often backfires. Instead, engagement should be sequenced into achievable steps.
Jim Milanowski put it plainly: too many referrals at once is too much. One clear next action is far more effective than five good ideas.
Theme: Progress happens one step at a time.
8. Trust and coalitions are the only way this scales
Finally, nearly every speaker returned to trust.
Kate Sawant, GM of Healthcare at Propel, highlighted how tools and data integration - especially across SNAP and Medicaid - create real opportunity, citing how Propel’s SNAP screener reached over a million users. But she was equally clear that delivery only works if paired with strong education and outreach.
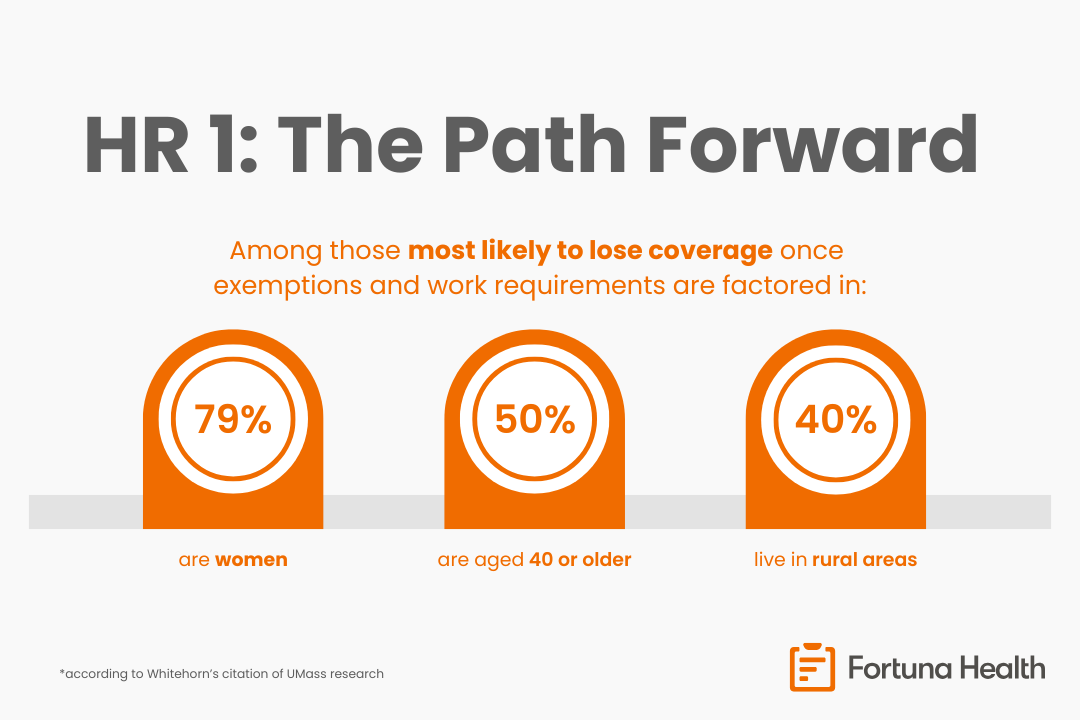
Jennifer Strohecker and Shelagh Kalland (Senior Director of Government Programs, External Relations at Blue Cross Blue Shield of Minnesota) emphasized that trusted intermediaries (e.g. providers, pharmacists, care coordinators, community leaders) are essential, particularly in rural areas and among people experiencing homelessness or language barriers.
Theme: Communications and outreach take a village.
Closing reflection
HR1 implementation will test systems, teams, and partnerships, but the greatest risk isn’t technical failure. It’s avoidable churn driven by confusion, overload, and misaligned processes.
What came through clearly at Medicaid Innovations is that success here won’t come from perfect compliance alone. It will come from intentional communication, trusted partners, and tools/technology built into workflows that meet members where they are.