Notes from IAMHP: Medicaid Leaders on Impacts of HR 1 and the Path Forward
At this week’s Illinois Association of Medicaid Health Plans conference, Healthcare and Family Services (HFS) Director Lizzy Whitehorn described HR 1’s legislation as “the biggest rollback to Medicaid since it began.” The federal changes facing Medicaid will reshape access, funding, and the future of care for millions - with Illinois particularly exposed to major fiscal and operational shifts.
PANEL:
- Moderator: David Vinkler, Vice President, IAMHP
- Elizabeth Whitehorn, Director, Illinois Department of Healthcare and Family Services (HFS)
- Paul Frank, Vice President, Government Relations, Sellers Dorsey
- Stephanie Myers, Director, State Affairs, Medicaid Health Plans of America (MHPA)
- Jill Hayden, CEO, Illinois Association of Medicaid Health Plans (IAMHP)
From Emergency Response to Implementation and Advocacy
Paul Frank of Sellers Dorsey reflected on the post-pandemic “roller coaster” - moving from emergency flexibilities of the unwinding to a new phase of federal restrictions and cost controls. The task ahead involves not only implementation, but also advocacy: ensuring policymakers understand the impact of these shifts on real people, providers, and the state’s healthcare infrastructure.
As several panelists noted, the coming years will test states’ ability to balance compliance with compassion - and to maintain stability while managing unprecedented federal retrenchment.
Eligibility, Operations, and IT Modernization
Illinois officials are working to maximize every available policy flexibility and exemption under HR 1 - including how “volunteering” and “work activities” are defined - to minimize harm and avoid unnecessary coverage loss.
Lizzy Whitehorn said the state is also leveraging IT automation to streamline eligibility renewals, improve customer experience, and support staff capacity. The Medicaid agency’s collaboration with the Department of Family Services, who co-administers the eligibility and IT systems, will be central to ensuring smooth implementation.
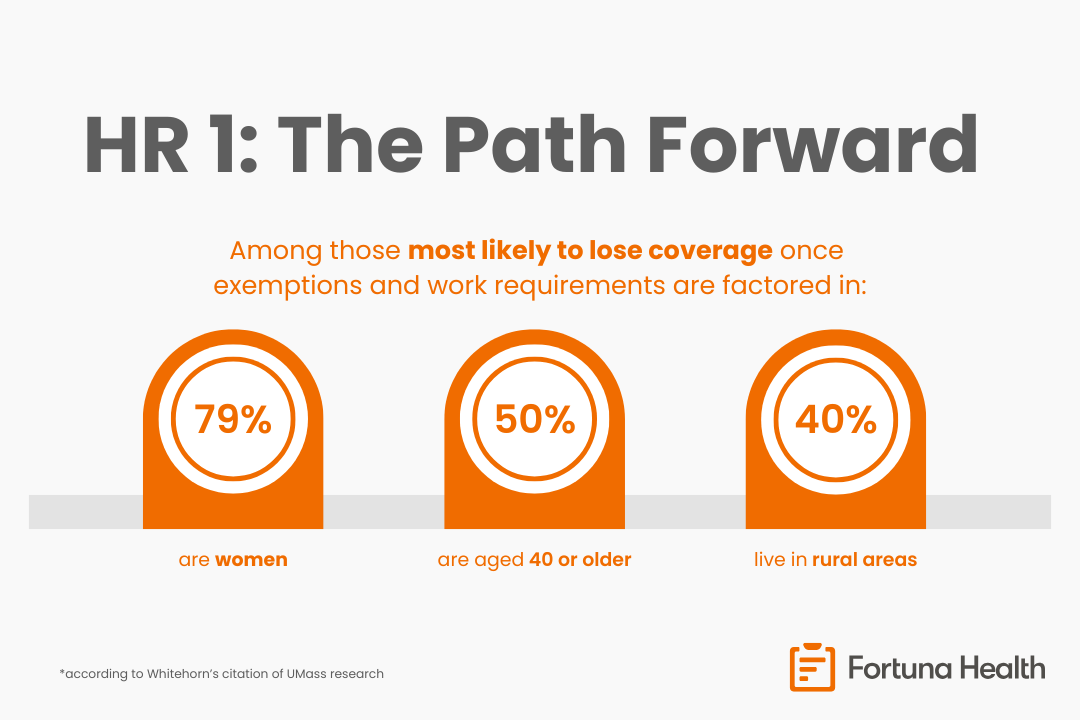
However, data limitations persist. Illinois does not currently collect detailed income data, making it harder to pinpoint who remains subject to the new requirements after exemptions are applied. According to Whitehorn’s citation of UMass research, among those most likely to lose coverage once exemptions and work requirements are factored in:
- 79% are women
- 50% are age 40 or older
- 40% live in rural areas
These data underscore that the policy’s burden will fall most heavily on older women and rural residents, individuals who often face barriers to meeting new reporting or work requirements despite serving vital caregiving and community roles.
Fiscal and Financial Pressures
KFF projects $880 billion in nationwide Medicaid reductions, including an estimated $2.8 billion in cuts for Illinois starting in 2028, escalating to over $6 billion as changes to provider tax and managed care rules take effect. Those reductions could translate to a 6% loss of the state’s annual Medicaid budget, significantly affecting provider payments, managed care plans, and network stability.
A new 3% cap on provider supplemental payments (SDPs) - covering both spending and revenue - will begin phasing in by 2028. While Illinois maintains a 4% reserve, speakers noted this won’t be enough to absorb the fiscal pressure.
Historically, states have delayed the most severe Medicaid cuts, such as the longstanding postponement of DSH payment reductions under the ACA. Panelists agreed a similar delay could happen again, but only if the Medicaid community organizes and speaks with a unified voice.
Plan Perspectives
Stephanie Myers of MHPA shared that states are already exploring provider rate reductions and MCO payment cuts to balance budgets. These measures may help close fiscal gaps on paper but risk undermining value-added services, care coordination, and provider network stability.
Plans are also increasingly concerned about provider participation - especially if lower reimbursement drives some providers to stop accepting Medicaid patients. This would create new challenges for MCO network compliance and member access.
MHPA is developing a policy brief to help states, plans, and advocates communicate with legislators and federal partners, emphasizing what Medicaid plans already do to manage costs and maintain quality. Myers said no major congressional changes to the HR 1 package are expected, making state-level advocacy even more critical.
The Safety Net Still Holds
Jill Hayden of IAMPH underscored that safety net providers will continue to bear the responsibility for care delivery, regardless of coverage shifts. She highlighted Illinois’ strong PHE unwinding campaign - which reminded residents to update their addresses, watch for mail, and respond to renewal notices - as a model for effective trusted-partner outreach.
That same infrastructure will be critical moving forward not only to preserve coverage, but to maintain the continuum of care. Hayden emphasized that the involvement of IL’s safety net providers are critical to minimize disruptions to screenings, vaccinations, home care, and follow-up services.
Fortuna Health’s Perspective: Partnership and Trust as Anchors
The lesson from the PHE unwinding is clear: trusted partners bridge policy and people. States can navigate this next phase of Medicaid change by strengthening collaboration with the ecosystem - plans, providers, and community-based organizations - and using data and technology to empower those partners to support meaningful outreach and enrollment actions.
Partnerships will be essential to:
- Maintain continuity of care as new policies roll out
- Communicate clearly with members and stakeholders through trusted local voices
- Support providers and plans as they adapt operationally and financially
- Use technology and automation to reduce administrative burden and improve the member experience