How States and Managed Care Plans Can Navigate Medicaid Work Requirements Together

The Challenge Ahead
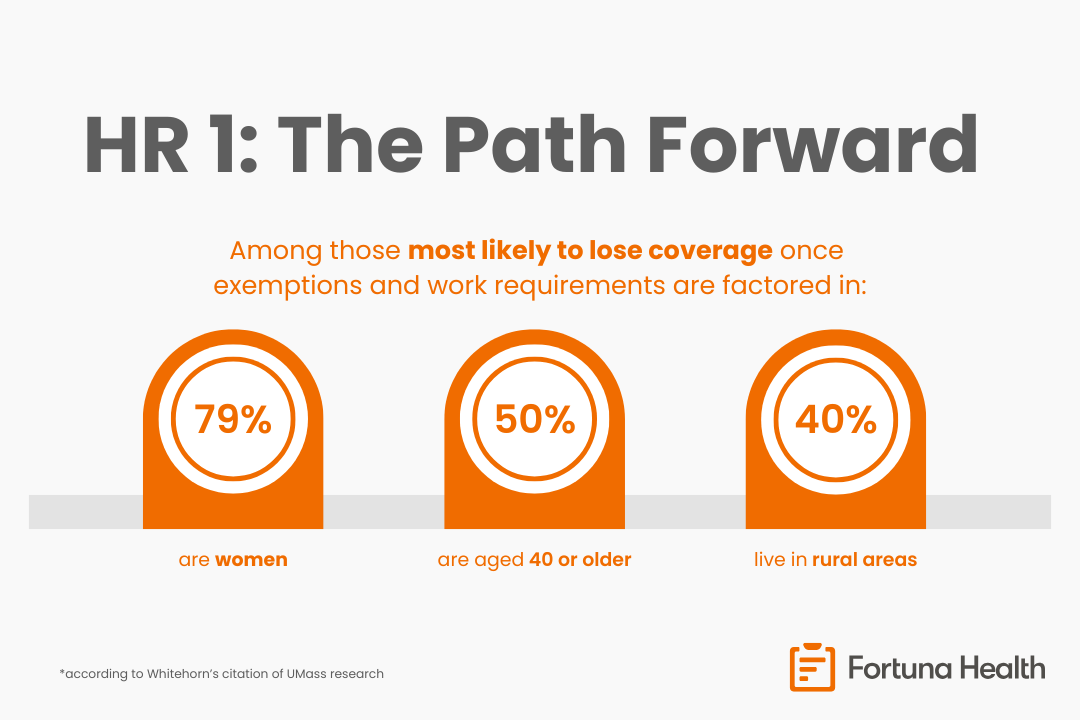
Beginning January 1, 2027, the OBBBA will require adults in the Medicaid expansion population to meet 80 hours per month of qualifying work activities or provide an exemption. Experts predict that millions of individuals could lose Medicaid coverage, and not because they fail to meet the requirements, but due to complex reporting systems.
As the National Health Program (NHeLP) highlights, states must now balance compliance with compassion: implementing the policy without destabilizing coverage for people who rely on Medicaid for essential care.
The Role of Managed Care Plans and Their Partners
Although OBBBA prohibits Medicaid managed care plans from formally determining compliance, these organizations remain crucial allies in education, outreach, and data-sharing. During the Covid-19 Public Health Emergency (PHE) unwinding, managed care plans successfully reconnected millions of members with state systems to prevent coverage loss, which is a playbook worth visiting now.
The new requirements will demand continuous, accessible communication between states and beneficiaries. Managed care plans play a critical role here, leveraging their trusted relationships and communication channels to reach members directly. Their outreach can matter even after a lapse: during the unwinding, up to half of disenrolled members were reinstated within 90 days at many plans, reflecting the impact of targeted follow-up and assistance. The deep community connections and member-level insights that they have can be used to design outreach campaigns that are accurate, timely, and human-centered. Beyond communication, managed care plans hold some of the most current and comprehensive data on member circumstances, which can help states identify individuals likely to qualify for exemptions to the work requirements. This kind of proactive identification not only supports compliance but prevents avoidable coverage interruptions that can have long-term health and financial consequences.
Fortuna believes the next phase of Medicaid policy demands the same spirit of partnership, strengthened by modern tools, interconnectivity, and member-centric engagement.
How Fortuna Helps
Fortuna Health works with states and managed care organizations to streamline eligibility, compliance, and communication workflows:
- Simplifies outreach and communication: Integrated workflows ensure members receive clear, multilingual notifications about work requirement steps or exemptions, reducing coverage loss due to missed deadlines
- Automates documentation and verification: Fortuna provides templates, affidavits, and auto-generated activity logs for employment, community service, education, or exemption categories, such as disability or caregiver status.
- Supports nontraditional and variable work: Fortuna’s specialty is handling seasonal, overtime, and gig work, which is critical for Medicaid members whose employment can be non-linear.
- Integrated verified income data: The platform connects to trusted income sources of truth (e.g. payroll, benefits, or self-employment records) to reduce the documentation burden on members and caseworkers alike.
By addressing both the policy and operational layers of the new requirements, Fortuna helps states and plans build systems that are compliant, compassionate, and efficient, protecting coverage while streamlining administration.
Acknowledgments and Sources
This companion brief builds on insights from the National Health Law Program’s article, “New Medicaid Work Requirements: How Managed Care Plans Can Help.”
Additional data regarding plan-led reinstatement comes from the Institute for Medicaid Innovation in its fact sheet, “2023–2024 Redetermination Survey Findings: Capturing the Impact of Redetermination.”